Bella Ramsey recently urged the NHS to consider adopting the term chestfeeding instead of breastfeeding, arguing that the language better reflects diverse family structures and acknowledges that not all mothers identify as women. The comment quickly sparked national discussion across healthcare, media, and social platforms.

Supporters interpreted the suggestion as an inclusive step toward recognizing transgender and nonbinary parents. They emphasized that language shapes access, comfort, and dignity within medical settings, especially for individuals who already face barriers when seeking support during pregnancy, birth, and early parenting experiences.
Critics, however, argued that breastfeeding is a medically established term tied to anatomy and public understanding. They worried that altering language might create confusion, dilute clarity in healthcare communication, and risk alienating mothers who feel represented by traditional terminology long used worldwide.
Healthcare professionals responded with mixed reactions. Some welcomed dialogue about inclusive language, while others stressed that consistent terminology remains essential for patient safety, research accuracy, and education. They noted that any change must carefully balance compassion with practical clarity across diverse clinical environments.
Ramsey clarified that the intention was not to erase anyone’s identity, but to expand recognition. According to supporters, the proposal aimed to ensure that no parent feels invisible when receiving guidance, encouragement, or medical advice during a deeply personal stage of life.
Advocacy groups for transgender parents praised the statement, sharing experiences of discomfort when medical language failed to reflect their realities. They argued that respectful terminology can reduce anxiety, strengthen trust with providers, and encourage earlier engagement with healthcare services during pregnancy and infancy.
Meanwhile, some women’s rights organizations expressed concern that replacing breastfeeding could unintentionally minimize the historical and biological experiences of women. They urged policymakers to consider whether inclusion can coexist with preserving language that many women feel represents their bodies and maternal identity.
Social media intensified the debate, often simplifying complex issues into emotional slogans. While some posts celebrated progress, others framed the conversation as a cultural conflict. Observers warned that polarized reactions risk overshadowing thoughtful discussion about healthcare communication and mutual respect.
Medical linguists noted that language evolves alongside society. They pointed out that many healthcare terms have changed over decades to reflect scientific understanding and cultural awareness. However, they emphasized that transitions require consensus, training, and careful implementation to avoid misunderstanding.
Parents from diverse backgrounds shared personal stories. Some welcomed chestfeeding as empowering, while others felt breastfeeding already included emotional, social, and nurturing meanings beyond anatomy. These contrasting experiences illustrated how a single term can carry multiple layers of significance.
NHS representatives acknowledged public interest but stressed that any policy changes would involve consultation with clinicians, patients, and advocacy groups. They highlighted the importance of evidence-based decision-making that considers inclusivity, clarity, and patient outcomes equally.
Cultural commentators suggested the debate reflects broader conversations about identity, language, and belonging. As societies become more diverse, institutions face increasing pressure to adapt communication while maintaining stability and trust within long-established systems of care.
Educators in public health encouraged respectful dialogue, reminding audiences that disagreements need not become personal. They argued that inclusive progress often begins with listening, understanding fears on all sides, and finding language that reduces harm rather than creating new divisions.
Some experts proposed compromise approaches, such as using both terms in appropriate contexts. They suggested that flexible language could respect individual identities while preserving familiar terminology in general communication, allowing patients to choose what feels most comfortable.
Others cautioned that too many terms might overwhelm patients, particularly those with limited health literacy. Clear explanations, they argued, remain more important than labels alone, ensuring that parents understand procedures, benefits, and support options during early childcare.
Ramsey’s statement also reignited discussion about celebrity influence. Supporters believe public figures can accelerate necessary conversations, while critics worry that simplified messages may overlook practical complexities faced by healthcare institutions serving millions of diverse patients.
Despite disagreement, many acknowledged that the debate itself reveals genuine concern for parental well-being. Both sides expressed desire for healthcare systems that feel respectful, accessible, and compassionate toward every family, regardless of identity or background.
Sociologists observed that language debates often symbolize deeper struggles over recognition. Words become markers of belonging, power, and visibility. Understanding this emotional dimension, they argued, helps explain why such discussions provoke intense and lasting public reaction.
Parents emphasized that regardless of terminology, support matters most. Access to lactation guidance, mental health care, and community encouragement often determines positive outcomes more than specific language choices used in official documents or educational materials.
Some voices urged patience, noting that cultural change rarely happens instantly. Institutions evolve gradually, learning from experience, feedback, and evidence. Open conversation, they said, remains healthier than rigid positions that leave little room for growth or compromise.
As discussion continued, many called for empathy toward all perspectives. They encouraged remembering that behind each opinion are personal experiences shaped by identity, health, history, and emotional connection to parenthood and family life.
Ultimately, the conversation surrounding chestfeeding and breastfeeding reflects society’s ongoing effort to reconcile tradition with inclusion. It challenges institutions to adapt thoughtfully while honoring those who feel represented by long-standing language.
Whether or not terminology changes, the debate has already highlighted the importance of respectful communication in healthcare. It reminds everyone that words matter, but so does the willingness to understand one another in an increasingly diverse and evolving world.
News
BREAKING NOW: A Sealed DNA Dossier Has Been Unearthed — Proving a 90-Year-Old Man Is Elvis Presley, and the Dark Truth Behind the 47-Year Cover-Up Is FAR MORE TERRIFYING Than His So-Called “Death”
In a revelation already shaking the foundations of music history and popular culture, a sealed DNA dossier has reportedly surfaced,…
“Besides her huge breasts, what else does she have? I can wear a headscarf and still attract attention. That’s the power of the eye.” Bella Ramsey criticized Sydney Sweeney for relying on her looks to get roles, claiming Sydney’s acting was SOULLESS.
A remark attributed to Bella Ramsey about beauty, attention, and acting standards recently circulated online, quickly igniting debate across entertainment…
When Florence Pugh first stepped into the Marvel spotlight, she said, “She protected me from day one,” as Scarlett Johansson quietly transformed Black Widow into a place where the pressure no longer felt… Her tone softened as Florence Pugh reminisced about those early days, admitting, “I didn’t feel as exposed as I expected,” before pausing without explaining what had
That was how Florence Pugh chose to describe her experience stepping into the Marvel Cinematic Universe — a world known for its…
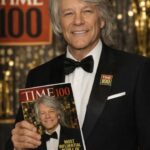
HISTORY SHIFTED THE MOMENT 2026 BEGAN—AND JON BON JOVI’S NAME LANDED WHERE LEGENDS LIVE.
HISTORY SHIFTED THE MOMENT 2026 BEGAN—AND JON BON JOVI’S NAME LANDED WHERE LEGENDS LIVE. TIME Magazine just nominated Jon Bon…
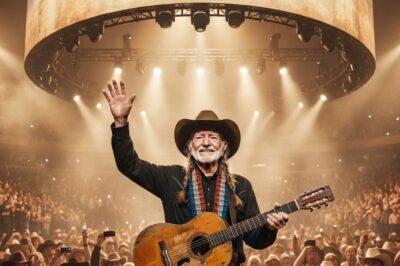
ONE LAST RIDE — AND WILLIE NELSON DIDN’T NEED TO SAY GOODBYE. The lights didn’t go dark all at once. They faded slowly. Like the end of a long summer evening. Willie Nelson stood at the center of the stage, 91 years old, his battered guitar resting against him like it had done for decades.
ONE LAST RIDE — AND WILLIE NELSON DIDN’T NEED TO SAY GOODBYE. The lights didn’t go dark all at once. They faded…
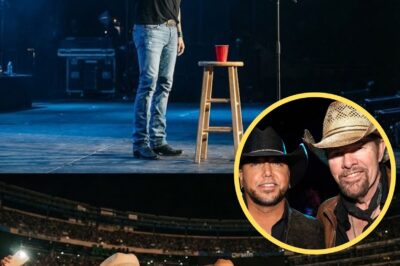
The microphone stand center stage was empty. A single red solo cup sat on the stool next to it. Jason Aldean walked out, but he didn’t pick up his guitar. He just stood there, looking at that empty spot. The opening chords of “Should’ve Been a Cowboy” began to play, but nobody sang. The crowd was confused for a heartbeat. Then, they understood. 50,000 people started singing. They took the verse. They took the chorus. They sang for the man who couldn’t be there. Jason didn’t sing a note. He just lifted that cup towards the sky. In the VIP section, grown men in cowboy hats were openly weeping.
The microphone stand at center stage was empty. No guitar leaned against it. No voice tested the sound. Just silence—and…
End of content
No more pages to load